The healthcare revenue cycle, a complex billing process, often starts with charge capture medical billing. This step is crucial for capturing, managing, and collecting patient service revenue.
If not managed accurately, it could lead to revenue leakage, over-coding charges, and non-compliant charges, leading to an expensive charge capture audit.
That’s why, to overcome the expensive billing procedure, we craft this guide exploring what is charge capture process, common challenges, and lastly, charge capture solutions to boost RCM.
Charge capture in healthcare is the process of documenting and recording the services provided to patients during their visits. Later, these service records are submitted to payers for reimbursement. Healthcare providers enter the charge capture healthcare data into a medical billing system or EHR to ensure they receive payment without any confusion or risk.
In a revenue generation context, the charge capture revenue cycle occurs after the clinical service is rendered and before a claim is submitted to the payer. In short, the revenue cycle charge capture acts as a bridge between clinical services and financial reimbursement for hospitals. Any sort of error in this stage leads to revenue leakage, underbilling, and compliance risks.
When specified in billing terms, the charge capture medical billing refers to a process that converts clinical notes, procedures, and delivered services into billable notes. These medical charge capture are coded using CPT, HCPCS, and ICD-10, but must be aligned with payer guidelines to ensure accurate and timely reimbursement.
Accurately capture the medical charges and submit to the payer for optimal revenue integrity, compliance, and cash flow optimization. Without proper charge capture, your practice will risk underbilling, delayed payments, and revenue loss. As evidence, entrust the data from HFMA, which indicates that hospitals in the U.S. lose about 1% of their net revenue because of hospital charge capture mistakes.
Hence, practices need timely and accurate charge capture medical billing, where all procedures, diagnoses, and treatments are accurately recorded. Additionally, physician charge captures need to follow payer guidelines. Such executions in medical billing result in correct billing, faster reimbursement, and prevent expensive audits or fraudulent claims.
Simplifying the charge capture process in medical billing involves delivering and documenting services, entering charges, verifying charge capture, and submitting charges to the payer for reimbursement. Following this strategic approach improves billing accuracy and ultimately increases revenue cycle in healthcare.
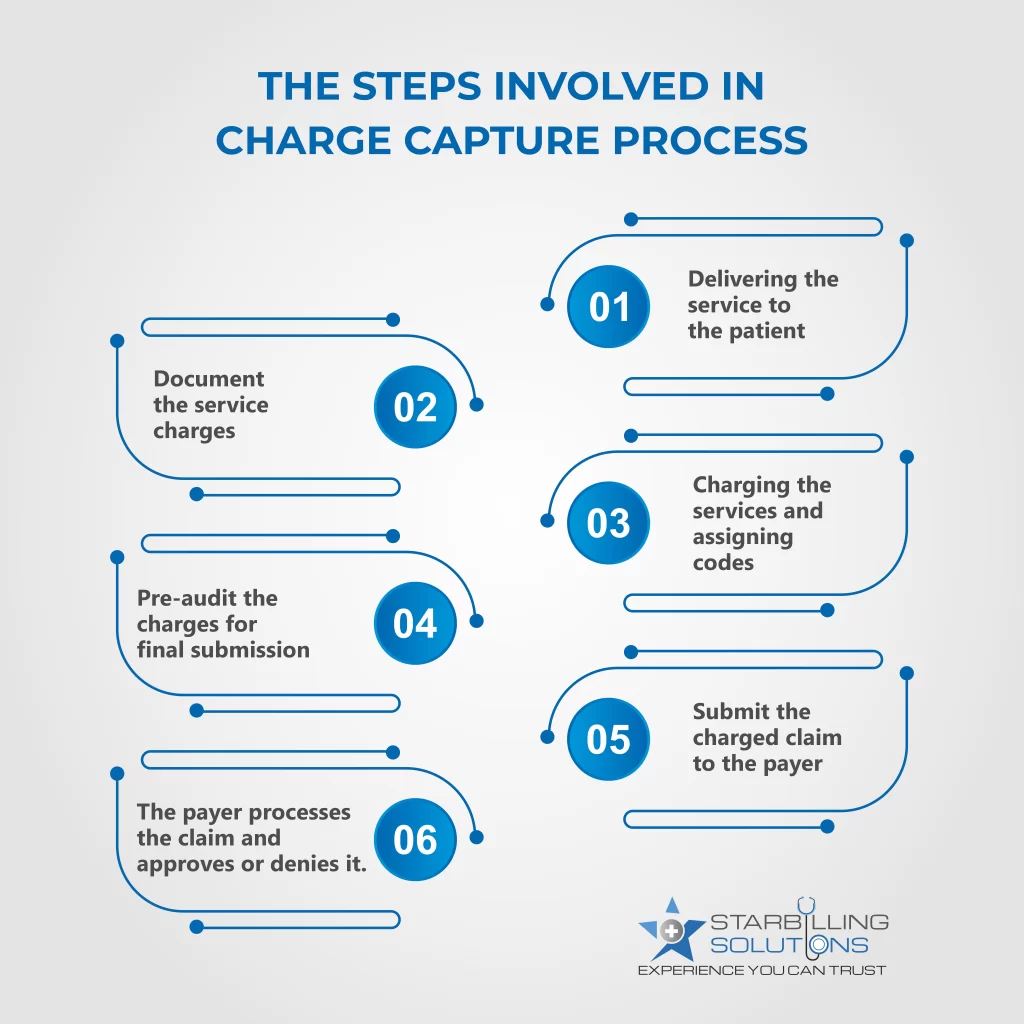
The patient visits the hospital or practice where the provider performs a medical service. The service could be a routine checkup, a critical surgery, or a laboratory test. The patient could also receive durable medical equipment, which is a prescription item for therapeutic purposes.
Then, the physician charge capture is documented for the rendered services. These records could include diagnosis, procedures, treatment, and supplies used in treatment. The documentation must be accurately billed to ensure a healthier revenue cycle.
Now, based on the documentation, the proper medical codes, such as CPT, ICD-10, and HCPCS, are assigned to those services. These codes identify the rates and complexity of the charged services.
The expert medical coding consultant or charge capture specialist will review the charges to make sure all data is accurate. This review team finds undercoded, overcoded, or missing documentation problems and corrects them for charge submission.
The verified charges are entered into the medical billing systems to generate a claim, which will be submitted to payers. Some practices still use manual billing, such as paper or printouts to draft data, which is time-consuming. However, most practices are embedded with Electronic health records and billing software, which automates the electronic charge capture and claim process.
The payer determines the charge capture in healthcare based on the corresponding medical codes and compliance with the payer. If approved, the company will reimburse the provider. If denied, the claim will be returned to the provider for correction and resubmission.
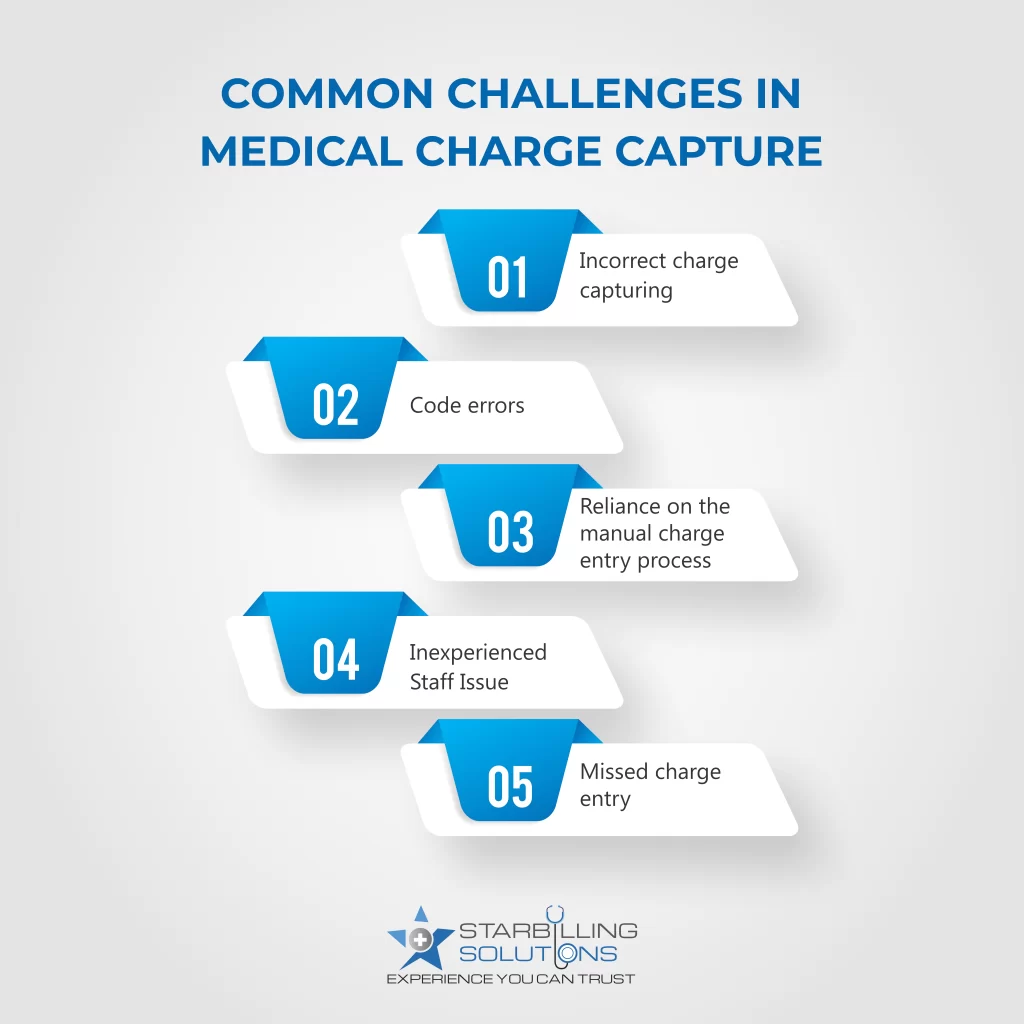
Providers often face common healthcare charge capture challenges, such as incorrect documentation, coding errors, manual entry reliance, and missing charge entries. All of these issues lead to claim denials, payment delays, and revenue loss.
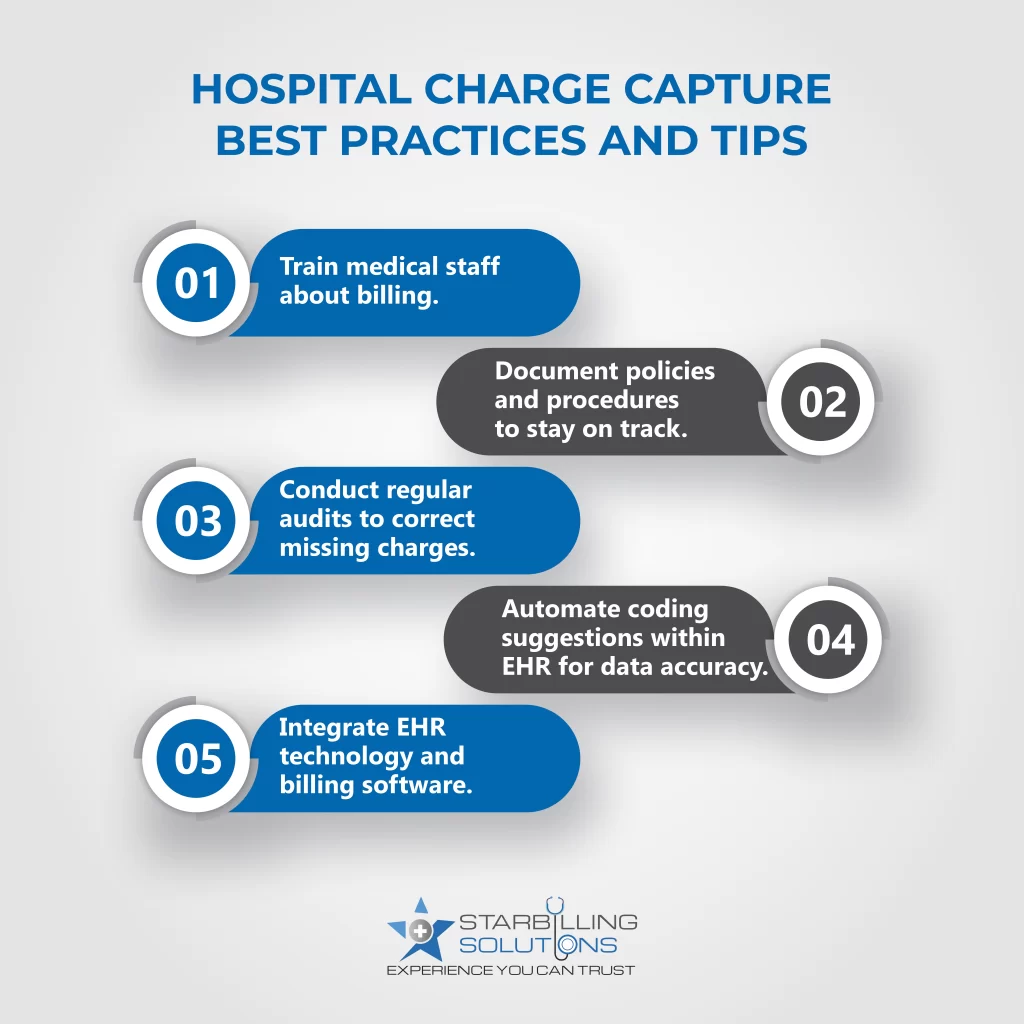
Capturing charge based reimbursement in medical billing involves best practices and tips such as training staff, regular audits, and integrating technology. By incorporating these strategies, providers ensure efficient and accurate charge collection.
Outrun the hours of administrative work and the frustration of charge lags by outsourcing SBS charge capture services. Our professionally driven charge capture solutions are designed to accurately and efficiently record services provided to patients. We offer charge capture medical billing solutions, including:
These solutions reduce administrative burdens, minimize errors, and ensure that no billable service goes unrecorded. So, without delaying further, partner with our medical billing agency today and experience a boost in your practice’s revenue.