Outsource Insurance Eligibility Verification Services
To Collect More Revenue And Decrease Claim Denials.
If you're a provider struggling with insurance issues, our healthcare insurance eligibility verification services are here to help. We know how time-consuming and frustrating it can be to confirm if a patient’s insurance is active and what it covers. That's why we offer quick and reliable medical insurance eligibility verification to make your practice easier. Say goodbye to endless phone calls and paperwork. With our health insurance verification experts, you can spend more time focusing on your patients and less time on admin tasks. Let us handle the insurance identification and higher coverage changes, so you don’t have to.

Get assurance for smoother operations and reduce errors with instant patient insurance eligibility verification checks. Say goodbye to tedious processes and hello to seamless, accurate verification in no time!
Now with our advanced health insurance verification system, you can uncover essential eligibility details with refined precision. This greatly reduces verification errors, speeding up claim processes. You'll find peace of mind knowing mistakes are minimized, helping you focus on delivering quality care while ensuring your patients are covered with confidence.
Get real-time updates on insurance eligibility for faster decision-making without any delays or guesswork. Quick feedback means you can plan better, address patient concerns effectively, and focus on the actual care instead of wasting time. By knowing insurance coverage instantly, you save time and build efficiency in your day-to-day operations.
Validate crucial patient insurance details upfront, so surprises like missed coverages or gaps don’t derail the claims process. It's all about being prepared rather than facing consequences later. When you avoid such disruptions proactively, patients feel reassured, and your workflow remains smoother and more predictable.
Streamline your insurance verification tasks efficiently, saving both time and resources while improving productivity. A smarter workflow reduces unnecessary costs and lets you handle multiple claims without added stress. The money and time saved can be better utilized elsewhere, like enhancing patient services or operational growth.
Enjoy smooth integration with your existing systems to ease the health insurance verification and eligibility process. There’s no need to worry about complicated setups or compatibility issues. With minimal effort and disruption, you can ensure accuracy, compliance, and continuity, all while improving user experience for your team.
Spot hidden issues early so claim denials become a thing of the past. A reliable verification process ensures approvals happen faster, saving time and resources, while ensuring patients receive their benefits without delay. You can avoid costly mistakes and boost success rates, building trust with both patients and insurance companies.
No more headaches with patient insurance eligibility verification details! This super-efficient process ensures that everything is checked and up to date, so you can focus on patient care without any issues. Here's how it all works:
Collect basic details during registration.
Verify plan and coverage details.
Ensure info is current with providers.
Update records for accurate billing.
Quickly verify insurance for urgent cases.
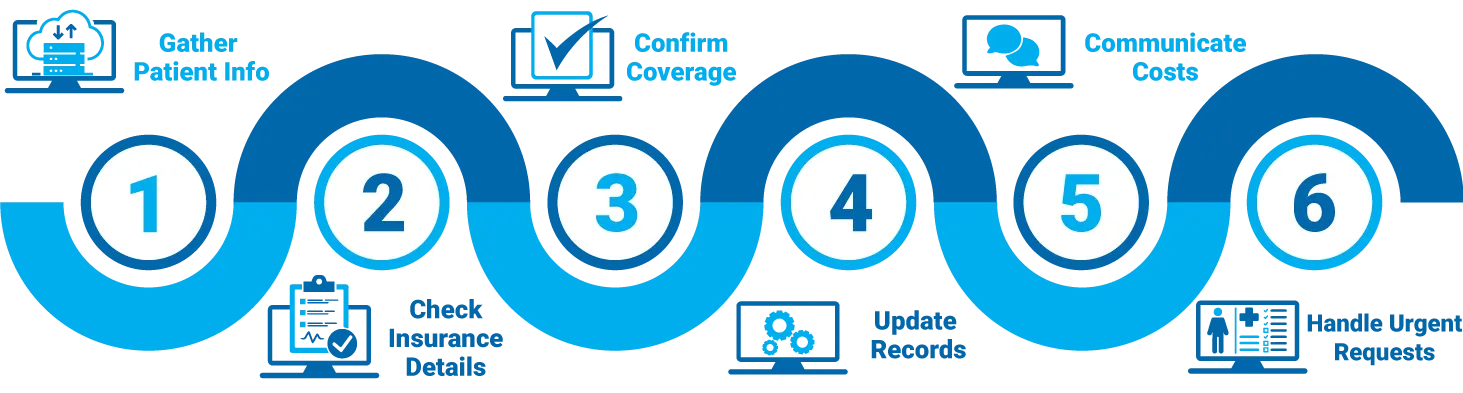

No more health insurance verification stress! Our easy and fast process makes sure everyone's covered, so you can get back to what you do best – caring for patients. Here’s how we do it in just four simple steps:
Collecting the basics: patient’s name, date of birth, and insurance details during registration. This is the foundation for verifying eligibility. We double-check the plan type, policy number, and coverage dates. By confirming all critical details, we ensure there are no surprises later.
We do cross-check with insurance websites or directly contact providers to ensure eligibility and benefits verification are up-to-date and accurate. This double-check process minimizes errors, improves trust, and ensures clients have correct coverage information at all times.
Updating our system with the verified details. This helps with smooth billing and quick access to necessary insurance information. It simplifies the claims process, reduces confusion, and helps healthcare teams focus on patients. To prevent delays, eliminate guesswork with accurate and updated records.
Use the verified insurance details to make claims processing simple and fast. This reduces errors, saves time, prevents delays, and helps in faster approvals, ensuring a smoother workflow for both patients and healthcare providers. Everyone benefits from better accuracy.
Customize Your Star Billing Solutions Experience Now!

Skip the lengthy insurance processes! With healthcare insurance eligibility verification services, you get quick and easy real-time insurance eligibility verification. Spend less time on paperwork and more time caring for your patients.
 Family Medicine
Family Medicine Physical Therapy
Physical Therapy Mental Health / Behavioral Health
Mental Health / Behavioral Health Laboratory Billing
Laboratory Billing Chiropractic Care
Chiropractic Care Telemedicine
Telemedicine Pain Management
Pain Management Dermatology
DermatologyI always dreaded the bottlenecks caused by insurance verifications. Since switching to this service, the real time insurance eligibility verification has been a game-changer. My admin staff spends less time on the phone, and claims are now processed swiftly and accurately.
Our practice was often plagued with billing errors due to incorrect insurance data. Thanks to the thorough health insurance eligibility verification, we've seen a significant reduction in claim denials. This service is indispensable for our practice.
Handling patient insurance details used to be incredibly time-consuming and frustrating. Now, with their efficient insurance verification and eligibility process, appointments and billing run more smoothly. This service has truly streamlined my practice operations.
Before outsourcing our insurance eligibility verification, we had a lot of confusion regarding patient coverage. This service has brought clarity and peace of mind. We can now focus on patient care without worrying about insurance issues.
I used to face constant interruptions to verify patient insurance details, which was very disruptive during busy hours. This healthcare insurance eligibility verification service provides accurate information quickly, allowing us to maintain our focus on patient care.