
We Provide the trustworthy Medical credentialing services to Empower Hospitals, Clinics, and Private Practices
Outsource with our authentic medical credentialing Services to stay compliant and focus on what truly matters - patient care. Don’t let administrative tasks slow you down. With our medical credentialing solutions, we verify and assess every physician’s qualification, training, experience, and licensure to meet the standards of your healthcare organization. Partner with our credentialing specialist today for a fast credentialing process.

Focus on providing the outstanding services for Health Care Credentialing. We accelerate your reimbursements with our professional credentialing services and solutions. Get authorized and reduce enrollment holds with insurance agencies.
We ensure credentialing services for providers are authenticated accurately and efficiently. By verifying their education, training, licensure, and certifications directly with issuing Authorities, we guarantee compliance with federal regulations. This approach accelerates credentialing and enrollment.
Simplifying the complex medical provider credentialing process with insurance networks, and other payer organizations. The comprehensive support of completion and submission of enrollment applications allows providers to start their practice without administrative delays.
We monitor and update provider credentials, anticipating changes and ensuring uninterrupted compliance with regulatory standards. This streamlines administrative processes and reduces the risk of non-compliance penalties, for high-quality patient care.
Get thorough support for obtaining hospital, clinic and practices privilege credentialing. Experts will manage the intricate credentialing requirements and accelerate the approval process, so providers can begin delivering care swiftly. This hassle-free service removes administrative burdens and enables excellent patient care.
The team assists healthcare providers and organizations through every step of the licensing process, covering physician, non-physician, DEA, EDI, ERA, EFT, CDS, CLIA, and group licensing. We manage applications, ensuring all documentation is complete and accurate for timely licence acquisition.
Leverages our industry expertise and data analytics to negotiate beneficial payor contracts for healthcare organizations. By securing favorable reimbursement rates and contract terms, we help maximize financial performance. Get ensured for the best possible terms, and enhanced profitability.
Streamline your Medical Credentialing Process with our experienced health care credentialing team. As a center of medical credentialing services we make sure the highest standards of compliance and help practices head and shoulders above their peers.
Gather all necessary documentation.
Investigate payer-specific requirements.
Fill out the credentialing application thoroughly.
Send in the completed application.
Regularly check the application status.
Confirm the application is reviewed and approved.
Finalize and sign agreements.
Continuously update and maintain credentials.
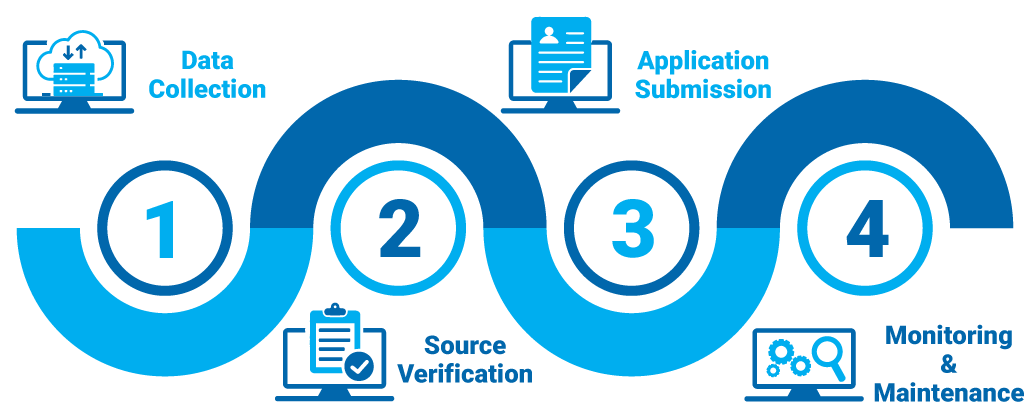

In the initial phase, we work with you to understand your specific credentialing needs and requirements. This involves discussing the type of practice, desired insurance network participation, and any unique preferences or priorities you may have.
Once we get all the initial requirements from your end, then we schedule a meeting of the provider with a medical credentialing specialist. The expert will lead throughout the process, and in a meeting, things will get clearer than ever before.
Once your requirements are clear, our dedicated credentialing specialists will start managing the process. They take over the comprehensive data collection, conduct primary source verification, and prepare your applications with extensive payer protocols.
After submissions, we maintain vigilant oversight of your credentialing applications with detailed tracking and reporting. You'll receive regular updates on the status of each application, ensuring transparency and accountability throughout the entire process.
Customize Your Star Billing Solutions Experience Now!

As professional Medical credentialing services, we track and report detailed record with standard regulations for more than 30 specialities.
 Family Medicine
Family Medicine Physical Therapy
Physical Therapy Mental Health / Behavioral Health
Mental Health / Behavioral Health Laboratory Billing
Laboratory Billing Chiropractic Care
Chiropractic Care Telemedicine
Telemedicine Pain Management
Pain Management Dermatology
DermatologyI thought I’d be stuck forever figuring out the credentialing process on my own. Luckily, your team made it so easy. I honestly don’t know what I’d do without your medical credentialing services—it feels like I finally have time for my patients again!
I was losing sleep over insurance credentialing for my practice. The constant paperwork was driving me nuts. But your service stepped in and handled everything. Now, I can finally rest easy knowing it’s all under control.
Managing billing and credentialing was becoming a nightmare for us. We needed a partner who could streamline it all, and your team delivered just that. The whole process was so smooth, and now we focus more on patients, less on paperwork.
I wasn't getting help from other healthcare credentialing companies, but your insurance service turned things around. Quick responses and real solutions—I wish I had found your team sooner.
The renewals were coming up, and I was clueless about what to do with my health care credentialing. Your team guided me through each step, making everything clear and straightforward. What a relief to have that kind of support!
Choosing the right partner for medical credentialing wasn't easy, but this team exceeded expectations. The peace of mind they provided allowed me to focus on growing my practice. Trusting them was the best decision.

Time to secure high-paying contracts and maximize revenue. We negotiate favorable terms with insurance payers, manage revalidation and credentialing, and audit reimbursement issues.
Optimize your revenue and focus on patient care