Ambulatory surgery centers (ASCs) offer a wide range of treatments and frequently have a large number of practitioners. However, they have a much smaller medical billing team to handle any queries or problems that may come up. The stress brought on by attempting to keep up with the intricate coding rules while operating a profitable surgery center is reduced when medical billing is outsourced to Star Billing Solutions. We work hard to outperform other ASC billing businesses and increase your payer payments
Although payments from insurance networks and public payers are rigid, ASC revenue can be significantly increased by securing favorable out-of-network provider rates. The process of obtaining the best prices is difficult, and payers have tenacious negotiators working for them. To guarantee that the greatest possible reimbursements are received for our ASC billing services, Star Billing Solutions has a trained negotiations team that is familiar with the procedure from start to finish.
Patient scheduling is the first step in the medical revenue cycle, and success in obtaining payments depends on completing this phase correctly. Our team of skilled ASC billing specialists will make sure that all necessary information is gathered during the intake and scheduling process and that it is accurately documented.
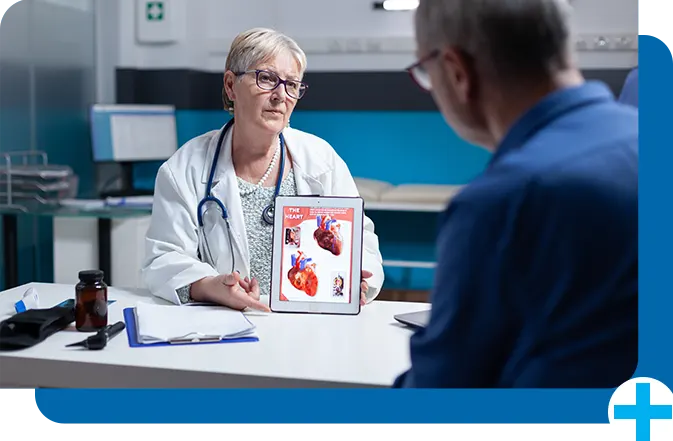
There are restrictions on what can be reimbursed for ambulatory surgical center billing, even if doctors in an ASC may conduct identical treatments at a hospital. Benefits verification is particularly crucial in that situation because the ASC will not be compensated if any treatment or operation is provided that is not on the approved list. The team of qualified experts at Star Billing Solutions ensures that suggested activities are covered by the patient's benefits, making the services offered reimbursable.
Even while all healthcare facilities utilize the same ambulatory surgery center billing codes established by the Centers for Medicare and Medicaid Services (CMS), surgical procedures usually call for specific modifiers. The entire claim will be rejected if a modifier is omitted or used inappropriately. Each claim is "scrubbed" by an experienced medical biller as part of Star Billing Solution’s normal operating procedure to make sure the coding information is accurate before the claim is filed.
Optimize your ambulatory surgery billing with accurate coding and timely claim submissions. We handle insurance complexities, reduce denials, and ensure faster reimbursements, so you can focus on patient care.
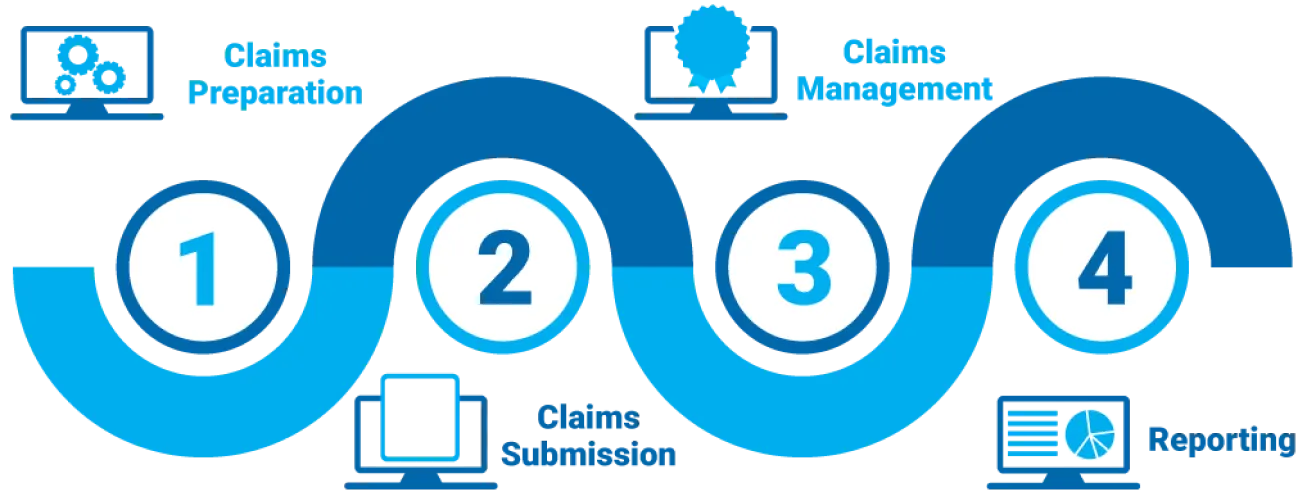
We ensure precise coding and timely claim submissions to maximize reimbursements.
We confirm patient coverage and obtain necessary approvals to prevent denials.
We handle claim rejections and submit appeals for quicker resolutions.
We streamline billing processes to improve cash flow and financial performance.
Customize Your Star Billing Solutions Experience Now!

 Family Medicine
Family Medicine Physical Therapy
Physical Therapy Mental Health / Behavioral Health
Mental Health / Behavioral Health Laboratory Billing
Laboratory Billing Chiropractic Care
Chiropractic Care Telemedicine
Telemedicine Pain Management
Pain Management Dermatology
DermatologyTheir billing expertise reduced our claim denials significantly, improving our revenue stream!
Fast approvals and accurate coding—our billing has never been smoother!
Their team handles everything efficiently, allowing us to focus on patient care!
When it comes to medical billing, trust is paramount. That's why we're grateful to have found this exceptional billing service. Their team's expertise is evident in every claim they process. They navigate the ever-changing billing landscape with finesse, ensuring our practice remains compliant and financially sound. A reliable partner indeed!