Urgent care centers need fast, error-free billing to keep revenue flowing. Our experts handle claims, coding, and denials, ensuring quick reimbursements. We stay compliant with evolving regulations, so you get paid on time. Focus on patient care while we manage the complexities of urgent care billing.
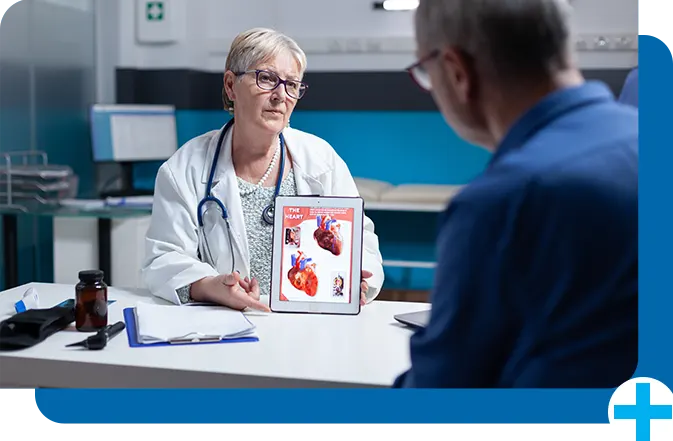
Connect demographic data with payer information and diagnosis codes for a streamlined process
Coding recommendations based on the latest regulations help providers and billers ensure claims are accurate and clean – speeding up reimbursement
The technologies to streamline billing operations include real-time insurance verification, EDI, ERA, EDT, card-on-file, and invoicing alternatives.
Our team is dedicated to following best practices, policies, and processes to reduce the burden associated with regulatory compliance and red tape.
Clinics frequently are unable to obtain the compensation they are due due to the complexity of urgent care billing, coding, payer contracts, and compliance. Receiving payment shouldn't be that difficult. Our billing for urgent care treatments can be helpful
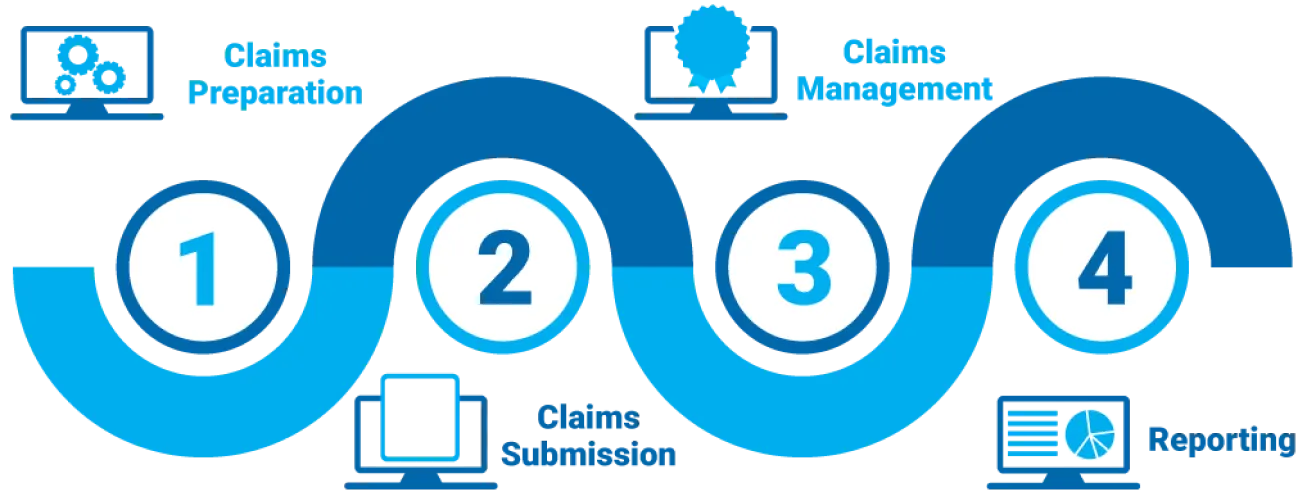
We ensure error-free coding and timely claim filing for faster reimbursements.
We confirm patient coverage upfront to prevent billing issues and claim denials.
We quickly identify and appeal rejected claims to maximize revenue recovery.
We maintain strict regulatory compliance and provide detailed financial reports for transparency.
Customize Your Star Billing Solutions Experience Now!

 Family Medicine
Family Medicine Physical Therapy
Physical Therapy Mental Health / Behavioral Health
Mental Health / Behavioral Health Laboratory Billing
Laboratory Billing Chiropractic Care
Chiropractic Care Telemedicine
Telemedicine Pain Management
Pain Management Dermatology
DermatologyOur revenue improved significantly with their urgent care billing expertise. No more delays or denials
They simplified our entire billing process, allowing us to focus on patient care. Highly recommend!
Fast, accurate, and professional billing services. Our collections have never been better!